|
 |
- Search
| Korean J Helicobacter Up Gastrointest Res > Volume 21(2); 2021 > Article |
|
Abstract
Anisakiasis is a fish-borne zoonotic disease caused in humans by the ingestion of raw or undercooked seafood infected by anisakid larvae. Anisakiasis usually causes abdominal pain, nausea, and vomiting. However, other symptoms, including dysphagia, heartburn, and chest pain, are rare. A 55-year-old woman presented to the emergency department for the evaluation of sudden-onset chest pain. The findings of the cardiology work-up were all normal. Upper gastrointestinal endoscopy revealed a nematode at the esophagogastric junction, which was successfully removed. The chest pain immediately subsided thereafter. Herein, we report a rare case of anisakiasis at the esophagogastric junction, which caused chest pain mimicking angina pectoris and was treated with endoscopic removal.
Anisakiasis in humans is a digestive disease caused by the larvae of nematodes belonging to the family Anisakidae. When sea fish or cephalopods in which larvae live are incompletely cooked and ingested by humans, the third-stage larvae invade the walls of the gastrointestinal tract and cause acute and chronic lesions [1,2]. Patients with anisakiasis usually present with symptoms such as abdominal pain, nausea, and vomiting, and other symptoms are relatively rare [3]. We managed a case of anisakiasis at the esophagogastric junction that was accidentally diagnosed due to chest pain. Chest pain is not a common symptom of anisakiasis; therefore, we report the case with a review of the literature.
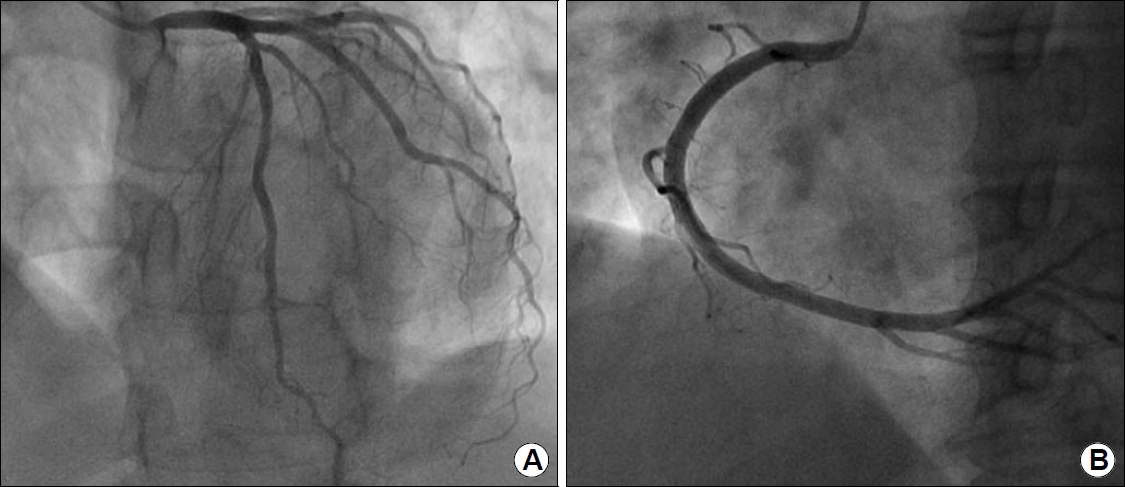
A 55-year-old woman with no specific past history other than hypothyroidism presented to the emergency room for the evaluation of sudden-onset chest pain. Chest pain occurred suddenly 1 day before and it was squeezing type of substernal pain, not accompanied by radiating pain, dyspnea, dysphagia, and regurgitation. Chest pain occurred at rest and lasted for about 10 seconds at first; however, its frequency and duration gradually increased. Vital signs were normal and there were no abnormal findings on laboratory tests including white blood cell count (10,000/mm3), eosinophil count (50/mm3), and serum cardiac markers, chest radiography, and electrocardiogram. Under suspicion of unstable angina, coronary angiogram was performed but the exam did not show any abnormality (Fig. 1). Therefore, she was referred to gastroenterology department to evaluate whether the cause of chest pain was of gastrointestinal origin. On upper gastrointestinal endoscopy, a whitish nematode was found penetrating the gastric mucosa just below the z-line, and it moved rapidly during examination (Fig. 2A, B). The nematode was removed through the scope using biopsy forceps, and it was confirmed as an anisakid larva (Fig. 2C). Chest pain immediately subsided after the endoscopic removal of the nematode. Additional history-taking revealed that she ate raw seafood, such as abalone and penis fish, 5 days before the symptom onset and that she had epigastric discomfort, several hours after taking raw seafood. One week after discharge, there was no recurrence of symptoms; therefore, outpatient follow-up was terminated.
Since anisakiasis was first reported in the Netherlands in 1960 [4], many cases of anisakis infection have been diagnosed in Korea, Pacific coastal countries and northern Europe where seafood consumption is high [1,5,6]. The adult-stage parasite lives mainly in the gastrointestinal tract of marine mammals, such as dolphins and seals, and the eggs are excreted into the sea through the feces of the definitive host. The excreted eggs develop into L1 stage larvae at a sea temperature of 2~27Ōäā. Then, these L1 larvae develop into L2 stage larvae when eaten by the first intermediate host, such as shrimp. L2 stage larvae develop into L3 larvae when eaten by the second intermediate host, such as fish, congers and cephalopods. Anisakiasis that occurs in humans is caused by L3 stage larvae that invade the human body through the second intermediate host (sea fish and cephalopods), that is eaten raw or improperly cooked [2,7].
Depending on the duration, infection can be classified as acute or chronic [2]. In most cases, edema occurs in the acute phase. Redness and erosion of the gastrointestinal mucosa can also be observed during endoscopy. Within 1 week of infection, embedded larvae can be detected in the wall of the gastrointestinal tract during endoscopy. However, over time, the characteristic endoscopic findings disappear because of the progression of inflammation. In chronic cases, abscess or eosinophilic granulation can be formed by larvae invading the mucosal layer. In our case, endoscopy was performed within 1 week after eating seafood, and the anisakid larva could be found.
Anisakiasis can also be classified according to the anatomical location of the infection. When 645 Korean anisakiasis cases were reviewed, the most common site of anisakis infection was the stomach (82.4%) [8]. In the case of acute gastric anisakiasis, typical symptoms include abdominal pain, nausea, and vomiting, which occur within 1~12 hours after eating raw seafood [2,8,9]. The small intestine is the second most common site of infection (11.4%).8 Acute anisakiasis of the small intestine causes symptoms similar to those of acute appendicitis and enteritis, such as acute lower abdominal pain, nausea, and vomiting. Small intestinal anisakiasis rarely causes intestinal obstruction [5,10]. Anisakiasis of the large intestine is rare (1.5%) [8], but mainly causes lesions in the cecum, sometimes breaking through the intestinal wall and invading the mesentery and pancreas [1,10]. Esophageal anisakiasis is very rare because the esophageal passage time of food is short. When anisakis invades the esophagus, atypical symptoms are exhibited; cases of swallowing difficulty [3] and heartburn [11] have been reported, and there have been two reports of esophageal anisakiasis presenting with chest pain in Korea [12,13].
The most effective treatment for anisakiasis is the removal of larvae after observation during endoscopy. However, in the case of small intestinal anisakiasis, since there is no generalized endoscopic method, drug administration can be considered. Although there are no widely proven effective drugs, albendazole (400 mg twice daily for 21 days) has been reported to be effective [14]. Therefore, prevention is the best treatment. To prevent human infection, it is necessary to keep the seafood frozen below -20Ōäā for 24 hours or more, or cook it above 60Ōäā to kill the larvae, and avoid eating raw seafood. In addition, anisakid larvae are usually found in the intestines of marine fishes; thus, removing the intestines immediately after capture can prevent the larvae from moving to the muscles [2].
We report a rare case of acute anisakiasis at the esophagogastric junction, which caused chest pain, mimicking angina pectoris, and was treated with endoscopic removal. Our case suggests that detailed history taking in a patient with chest pain could prevent unnecessary invasive examination such as coronary angiogram. Although rare, acute anisakiasis at the esophagogastric junction should be considered a possible cause of acute chest pain, especially in regions where fish is commonly consumed raw.
Acknowledgements
This work was supported by clinical research grant from Pusan National University Hospital in 2021.
REFERENCES
1. Cho EY, Song WK, Ahn YH, et al. Anisakiasis of the colon: report of two cases. Korean J Gastrointest Endosc 2006;32:298ŌĆō301.
3. Brieau B, Rahmi G, Benosman H, Cellier C. Acute dysphagia and odynophagia revealing an unusual case of oesophageal anisakiasis. Dig Liver Dis 2015;47:e21.


4. van Thiel P, Kuipers FC, Roskam RT. A nematode parasitic to herring, causing acute abdominal syndromes in man. Trop Geogr Med 1960;12:97ŌĆō113.

5. Ko GH, Park CK, Kong HJ, Choi CS, Lee SH, Hong SJ. Intestinal anisakiasis. Korean J Pathol 1988;22:154ŌĆō158.
6. Song TJ, Cho SW, Joo KH. Endoscopic findings of acute gastric anisakiasis: thirty-nine cases in Inchon City. Korean J Gastrointest Endosc 1999;19:878ŌĆō884.
7. Lee DH, Cho SW, Shim CS, et al. Ileal anisakiasis: a case report. Korean J Gastroenterol 1989;21:639ŌĆō644.
8. Sohn WM, Na BK, Kim TH, Park TJ. Anisakiasis: report of 15 gastric cases caused by anisakis type I larvae and a brief review of Korean anisakiasis cases. Korean J Parasitol 2015;53:465ŌĆō470.




9. Lee EJ, Kim YC, Jeong HG, Lee OJ. The mucosal changes and influencing factors in upper gastrointestinal anisakiasis: analysis of 141 cases. Korean J Gastroenterol 2009;53:90ŌĆō97.

10. Kim HJ, Park C, Cho SY. A case of extragastrointestinal anisakiasis involving a mesocolic lymph node. Korean J Parasitol 1997;35:63ŌĆō66.



11. Uehara A, Okumura T. Esophageal anisakiasis mimicking gastroesophageal reflux disease. Am J Gastroenterol 2017;112:532.


12. Park TG, Lee DH, Lee JS, et al. A case of esophageal anisakiasis. Korean J Gastrointest Endosc 1999;19:597ŌĆō600.
13. Shin KD, An CM, Nam SW, et al. A case of esophageal anisakiasis presenting as chest pain mimicking angina. Korean J Gastrointest Endosc 2007;35:19ŌĆō22.
-
METRICS

-
- 1 Crossref
- 2,472 View
- 51 Download
- Related articles in Korean J Helicobacter Up Gastrointest Res
-
Treatment of Adenocarcinoma of the Esophagogastric Junction2012 September;12(3)