An Esophageal Squamous Cell Carcinoma with Lymph Node Metastasis Presenting as a Small Subepithelial Tumor
Article information
Abstract
A subepithelial tumor-like esophageal carcinoma is rare. We report a case of an esophageal squamous cell carcinoma with lymph node metastasis presenting as a small subepithelial tumor. A 68-year-old man presented to our hospital complaining of hoarseness since last three months. Endoscopic examination revealed a 1 cm hard and fixed subepithelial tumor with surface erosion in the lower esophagus. A biopsy specimen was obtained using conventional forceps, and histopathological evaluation revealed few atypical squamous epithelial cells. Subsequent EUS demonstrated a homogeneous hypoechoic lesion in the deep mucosal layer. A CT scan of the chest showed a 3 cm mass in the right upper paratracheal area. EUS-guided fine needle biopsy of the lesion led to the diagnosis of squamous cell carcinoma with lymph node metastasis.
INTRODUCTION
Esophageal cancer is associated with a poor prognosis and exceptionally a low survival rate. Although esophagectomy remains the standard treatment for localized esophageal cancer, there is considerable morbidity and mortality associated with surgery [1]. Endoscopic resection has been widely used for the treatment of superficial esophageal squamous cell carcinomas based on favorable outcomes [2,3]. Therefore, early detection and timely treatment are important to improve clinical outcomes of esophageal cancer.
Since esophageal cancers originate from the epithelial layer of the esophagus, most accompany mucosal abnormality. Therefore, endoscopic examination with biopsy is the gold standard for diagnosis of esophageal cancer [4]. Advanced esophageal cancers usually present as a mass or ulceration, which can be easily recognized during endoscopic examination. Endoscopic diagnosis of superficial neoplasia can be challenging, as they appear as subtle and flat hyperemia or granular change of the esophageal mucosa. Nonetheless, esophageal cancer rarely grows in a subepithelial tumor (SET)-like pattern. Here, we report a case of esophageal squamous cell carcinoma with lymph node metastasis presenting as a small SET.
CASE REPORT
A 68-year-old man visited the otolaryngology department with complaints of hoarseness lasting since three months. He had been diagnosed and prescribed for high blood pressure. He was a never-smoker but had a history of habitual alcohol drinking for 50 years. He was otherwise in good health, with no history of gastrointestinal symptoms. Vital signs were stable and laboratory test results were unremarkable.
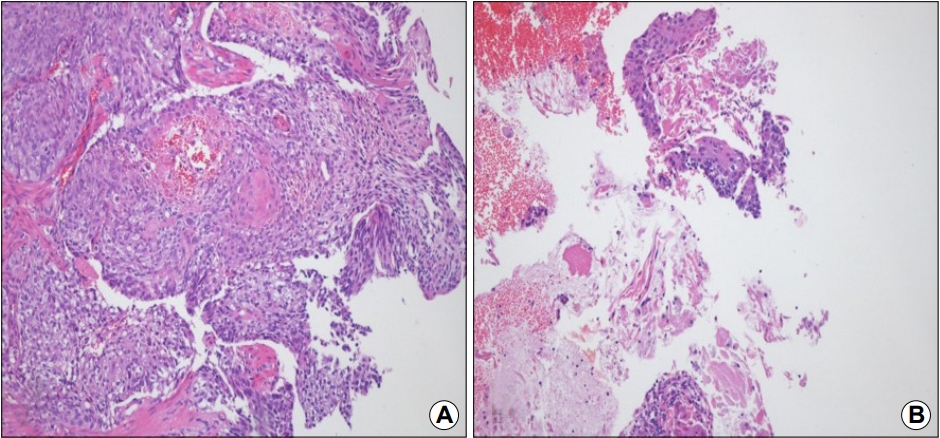
During laryngological examination, right vocal cord palsy was noted. The patient was referred to the department of gastroenterology for endoscopy. Endoscopic examination revealed a 1 cm hard and fixed esophageal SET with surface erosion 36 cm away from the upper incisors (Fig. 1). Forceps biopsy specimens were obtained from the mucosal lesion, and histopathological evaluation showed few atypical squamous epithelial cells. EUS using a 20 MHz mini-probe demonstrated a circumscribed homogeneously hypoechoic lesion in the deep mucosal layer. Repeat biopsy with standard forceps was performed, which resulted in the diagnosis of squamous cell carcinoma.
(A, B) White light endoscopy and narrow-band imaging show a subepithelial lesion in the lower esophagus. There is erosion on the surface of the lesion. (C) The lesion is fixed and hard when pressed with forceps. (D) EUS show a homogeneous hypoechoic lesion in the deep mucosal layer.
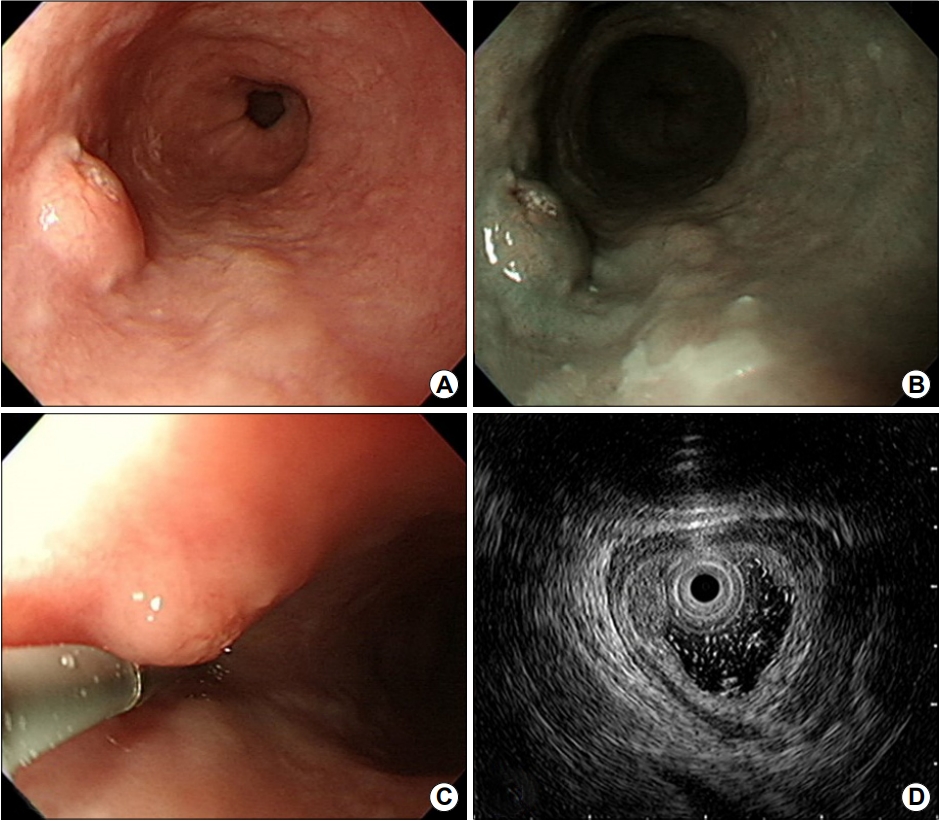
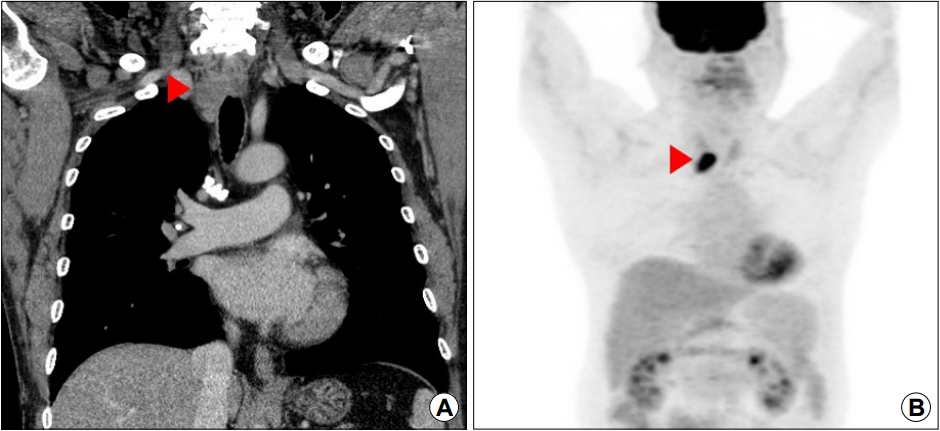
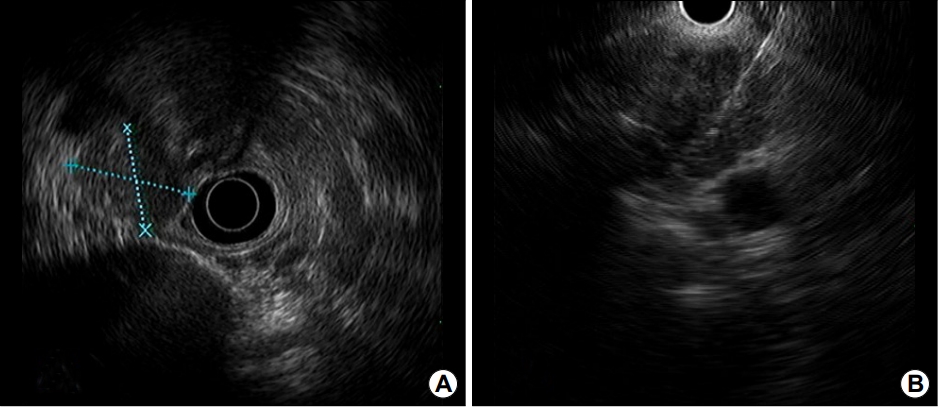
Subsequently, imaging studies for staging were performed. CT scan of the chest and positron emission tomography revealed an approximately 3 cm mass in the right upper paratracheal area (Fig. 2). EUS-guided fine needle biopsy (EUS-FNB) was performed (Fig. 3). The histopathological diagnosis was squamous cell carcinoma, and palliative chemoradiatiotherapy was adopted (Fig. 4).
(A) A CT scan show a 3 cm mass in the right upper paratracheal area (arrowhead). (B) A positron emission tomography scan of the corresponding lesion show hypermetabolic activity (arrowhead).
(A) EUS shows a 25.4×21.6 mm heterogeneous hypoechoic mass in the right upper paratracheal area. (B) A EUS-guided fine needle biopsy is performed.
DISCUSSION
SETs are usually encountered incidentally during endoscopic examination [5]. The differential diagnosis of SETs includes both benign and malignant neoplasms, including leiomyoma, granular cell tumor, and gastrointestinal stromal tumor [6,7]. Lymphoma or metastatic tumor can appear as SETs, and epithelial tumors rarely present SET-like appearance [8]. They closely mimic the mesenchymal tumors on EUS, and carcinomas of SET-like growth may be of the poorly differentiated or undifferentiated type [8].
SET-like pattern is a rare presentation of esophageal cancer [9-13]. In a previous study, the authors reported a case of advanced squamous cell carcinoma with multiple lymph node metastasis initially found as a 1 cm esophageal SET [10]. Small surface erosion was observed on endoscopy; however, a biopsy specimen could not be taken because of poor cooperation of the patient. Endoscopic resection of the primary lesion was performed and subsequent surgery revealed advanced esophageal cancer infiltrated into the adventitial layer. In another case report, an approximately 0.8 cm esophageal SET was noted, and the presumed diagnosis was leiomyoma based on the endosonographic features [11]. The final diagnosis was made after endoscopic resection of the tumor, which was esophageal squamous cell carcinoma invading the submucosal layer without lymph node metastasis. In these cases, the primary lesions were relatively small (less than 1 cm) and they appeared as circumscribed hypoechoic lesion confined to mucosal and submucosal layers, suggesting the possibility of mesenchymal tumor. The diagnosis could not be made without clinical suspicion and endoscopic resection.
There have also been reports of intramural squamous cell carcinomas, which presented as esophageal SET with completely normal overlying mucosa [12,13]. In these cases, the primary cancer was located mainly in the submucosa, and had initially been suspected of being SET. Endoscopy and radiological investigations could mislead to a diagnosis of SET rather than esophageal cancer due to the nonsuspicious appearance of the overlying mucosa.
Our case differs from those reported earlier because the endoscopic forceps biopsy was useful to make a definite diagnosis. During endoscopic examination, it is recommended to perform forceps biopsy on the mucosa overlying the SET [8,14]. However, for most SETs, the results of standard forceps biopsy, in which tissues are obtained from across the epithelium that covers the tumor, are not diagnostic, even with large-capacity forceps or bite-on-bite technique; this is primarily because of its limited depth of penetration [15]. In contrast, forceps biopsy may help reach a definitive diagnosis when there is a mucosal abnormality, such as surface erosion, changes to the vasculature, or ulceration. Therefore, meticulous evaluation and clinical suspicion are important. Image-enhanced endoscopy or chromoendoscopy with Lugol staining can be helpful for the detection and delineation of squamous cell neoplasm. In addition, repeated biopsy or endoscopic resection should be considered if malignancy is suspected.
EUS enables to characterize SETs, including the size, layer of origin, delineation, and echogenic pattern of the lesions [16]. Current guidelines recommend that asymptomatic SETs smaller than 2 cm or having typical EUS features of benign disease can be periodically assessed [8,14]. When SETs have clinically malignant features on endoscopy, such as irregular borders, ulceration, or growth during endoscopic follow-up, a histological diagnosis should be attempted to determine the optimal treatment strategy. Tumors confined to the mucosal and submucosa layers can be resected endoscopically. EUS-guided tissue sampling, such as EUS-guided fine needle aspiration (EUS-FNA) or EUS-FNB, provides adequate tissue samples for both histopathological and immunohistochemical analyses, particularly for those originated from the proper muscle layer [17]. Several factors may contribute to the diagnostic performance of EUS-guided tissue acquisition, including the size and location of the lesion, needle size and type, sampling techniques, and utilization of on-site cytopathologist [18]. In a previous report, which investigated the diagnostic accuracy of EUS-FNA in esophageal SETs, 47.7% of tissue samples were considered insufficient or nondiagnostic [6]. In addition, the diagnostic yield of EUS-FNA was lower for small SETs less than 2 cm [19]. Every method of tissue acquisition has its limitation, and the choice of method for tissue diagnosis in SETs should be based on various factors.
In conclusion, an esophageal SET can be an atypical presentation of esophageal cancer, which should not be overlooked. Timely identification of this feature of the esophageal cancer is necessary for appropriate evaluation and management.
Notes
No potential conflict of interest relevant to this article was reported.