Esophageal Subepithelial Lesion in a Patient with Painful Swallowing
Article information
Question: A 41-year-old female patient visited the clinic complaining of non-progressive dysphagia, odynophagia, and postprandial epigastric pain lasting approximately 1 month. Otherwise, she was in good health and reported no other symptoms, including weight loss, fever or productive cough.
Esophagogastroduodenoscopy showed an about 2.0-cm sized subepithelial lesion at 25~27 cm from the incisor teeth (Fig. 1A). This lesion was accompanied by a linear ulcer on the surface (Fig. 1B). Furthermore, chest CT showed a protruding luminal lesion in the medial wall of the mid-esophagus (Fig. 2A) and necrotic lymphadenopathy in the subcarinal area, which compressed the esophageal lumen (Fig. 2B).
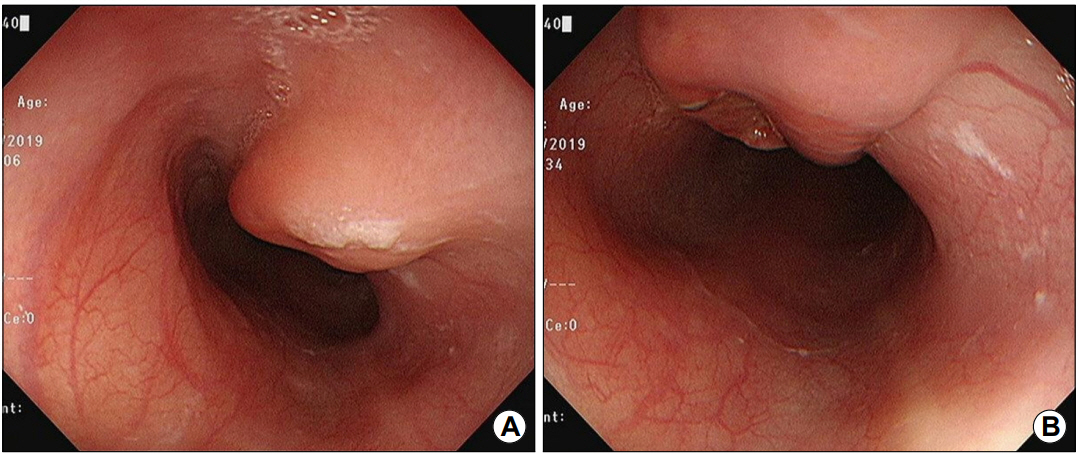
Endoscopic findings showing (A) a 2.0-cm-sized subepithelial lesion on the mid-esophagus, with (B) ulceration on the surface.

Initial chest CT findings showing (A) a protruding luminal lesion on the mediolateral wall of the mid-esophagus (arrow) and (B) necrotic lymph node in the subcarinal area (arrowheads).
What is the most likely diagnosis?
Answer: The endoscopic biopsy specimen obtained from ulcer of the lesion revealed vague granulomatous inflammation involving epithelioid histiocytes and lymphocytes in the stroma, pathologically suggesting tuberculosis. The result of acid-fast bacillus smear was negative, but the molecular nested PCR study for Mycobacterium tuberculosis was positive.
The patient underwent the first 2-month therapy for tuberculosis with isoniazid, pyrazinamide, rifampin, and ethambutol. Two months after anti-tuberculosis treatment, her symptoms of dysphagia disappeared, and odynophagia improved. Despite the doctor’s recommendation, she refused repeated endoscopy. After another 4 months of medication, no symptoms or clinical signs remained. The repeated CT revealed no lesion in either esophagus (Fig. 3A) or subcarinal area (Fig. 3B).

Follow-up chest CT findings. (A, B) The previous protruding lesion in the mediolateral wall of the midesophagus and the necrotic lymph node in the subcarinal area are no longer visible.
Esophageal tuberculosis is a rare disease. Usually, it occurs as a result of direct extension of infection from mediastinal nodes, rarely the infection by spread from the lungs or bloodstream. Considering that Korea has a high prevalence of tuberculosis, the differential diagnosis of esophageal ulcerative, or mass-like lesions, practically subepithelial mass type at the mid-esophagus, should include esophageal tuberculosis [1]. If esophageal tuberculosis is suspected, it can be diagnosed by endoscopic biopsies or postoperative pathology. However, multiple endoscopic biopsies often show only nonspecific chronic inflammation. If satisfactory findings are not found on the biopsy, esophageal tuberculosis should be differentiated by the detection of acid-resistant bacteria or by Mycobacterium tuberculosis PCR [2]. Although chest CT can help to find the primary site of tuberculosis, to determine lymphadenopathy or the presence of pulmonary esophageal fistulas, and to differentiate from malignant tumors of the esophagus, they cannot confirm esophageal tuberculosis. Lymphadenitis in the subcarinal area is one of the most common CT findings which patients with esophageal tuberculosis have [3]. Since typical histological findings of this disease are rare in real practice, it is necessary to evaluate the clinical features, radiological and endoscopic findings, and response to anti-tuberculosis drugs to diagnose esophageal tuberculosis.
Notes
No potential conflict of interest relevant to this article was reported.
