 |
 |
- Search
| Korean J Helicobacter Up Gastrointest Res > Volume 23(1); 2023 > Article |
|
Abstract
Background/Aims
Esophageal perforation is associated with high mortality and morbidity in patients presenting to the emergency department (ED) with esophageal injury. We investigated the effectiveness of initial CT scan in patients with esophageal injury to determine the risk factors for complications.
Methods
Patients admitted through the ED for evaluation of esophageal injuries between January 2001 and May 2020, were investigated. Demographic data, etiological factors, comorbidities, treatment administered, and outcomes were collected. Esophageal injury was graded based on the following CT criteria: (a) normal, (b) pneumomediastinum, (c) mediastinitis, fluid collection, abscess, or overt esophageal wall injury, and (d) pleural effusion, subcutaneous emphysema, or pneumothorax. Grade 2 was defined as microperforation and grades 3 and 4 as overt perforation.
Results
Of 281 patients with esophageal injury, 38 had CT-documented overt perforations and 20 had microperforations. Foreign body-induced injury (n=37), Boerhaave syndrome (n=12), and chemical injury (n=3) were common causes of esophageal injury. Complications occurred in 24 (8.5%) patients. Risk factors for complications were age Ōēź65 years (OR 4.14, 95% CI 1.18~14.56, P=0.027), cerebrovascular disease (OR 8.58, 95% CI 1.13~65.19, P=0.038), Boerhaave syndrome (OR 12.52, 95% CI 2.07~75.68, P=0.006), chemical injury (OR 15.72, 95% CI 3.67~67.28, P<0.001), and CT-documented grade 4 perforation (OR 15.75, 95% CI 4.39~56.55, P<0.001).
Esophageal perforation is a rare clinical emergency associated with high mortality and morbidity [1]. The incidence of esophageal perforation is reported in 3~10 cases per 100,000 people [2]. With recent advances in endoscopic and surgical technology, the landscape of esophageal perforations is changing rapidly [3]. Though it is a rare condition, a relatively large number of patients can be at risk for esophageal perforation after foreign body ingestion, esophageal trauma or chemical injuries [4]. In patients presenting with esophageal injury to the emergency department (ED), initial clinical decision-making is important for anticipating upcoming esophageal complications and outcomes.
Esophageal perforation can cause various complications according to the mechanism, extent, and location of the perforation. Many organs including the bronchus, trachea, heart, and lungs, multiple vertebral levels surround or share a vertical course with the esophagus. Owing to its anatomical characteristics, diverse complications can arise from esophageal perforations [5,6].
There are several studies on the causes and risk factors for esophageal perforation [1,7]. However, studies on the mortality according to the management of esophageal perforation are limited [8]. Asian foods often contain fish and chicken bones, increasing the risk of foreign body intake. Therefore, the main cause of esophageal perforation differs from that in the West where the main cause is iatrogenic [9]. Patients with esophageal injury should undergo a chest CT scan if trauma or perforation is suspected. However, they are currently performed only in some cases of foreign body-induced esophageal injury in the ED, which is one of the most common causes. The early identification of patients who are at risk of esophageal injury progression is a major hurdle in the ED.
This study aimed to identify the clinical factors and severity on CT scans that are associated with severe complications in patients who presented to the ED with esophageal injuries. In addition, we investigated the risk of complications caused by esophageal injury based on these factors.
All patients diagnosed with esophageal injury between January 1, 2001 and May 31, 2020, were identified using three diagnostic mechanisms. Potential cases were identified as having one or more of the following International Classification of Diseases 10 diagnostic codes: T179 (foreign body aspiration), T172 (foreign body in the throat or pharynx), T181 (foreign body in the esophagus), and K223 (Boerhaave syndrome and esophageal perforation). Second, we linked the list of all the patients who had undergone chest CT at the ED. Finally, two trained gastroenterologists (JRB and ESJ) performed a detailed chart review to increase the specificity and ensure suitable cases. The exclusion criteria were as follows: (i) patients who had iatrogenic esophageal injuries during the hospital stay and (ii) suspected upper gastrointestinal bleeding due to esophageal injury (Fig. 1).
Data collected for each patient included sex, age, comorbidities, causes, treatment, and outcomes. We investigated the following comorbidities for associations with perforation: (i) hypertension, (ii) diabetes mellitus, (iii) cardiac disease, (iv) chronic liver disease, (v) chronic renal disease, (vi) chronic lung disease, and (vii) cerebrovascular disease. We reviewed the clinical records, including pathology (esophageal perforation confirmation on gross pathology), endoscopy, chest CT, chest radiography, abdominal radiography, gastrografin esophagography reports and surgical records. Radiological reports were obtained and confirmed by experienced radiologists. The white blood cell (WBC) and C-reactive protein (CRP) values in the initial blood test were evaluated for association between initial inflammation and esophageal injury. This study was approved by the Ewha Womans University Mokdong Hospital Institutional Review Board (No. 2020-02-31). As this was a retrospective study, the requirement for informed consent was waived.
We evaluated the initial chest CT scan findings performed after presenting to the ED. We graded the CT scans according to the following criteria [4,10]: grade 1: normal; grade 2: pneumomediastinum (small air bubbles adjacent to the esophagus); grade 3: mediastinitis, fluid collection, abscess, and overt esophageal wall injury; grade 4: pleural effusion, subcutaneous emphysema, and pneumothorax.
Grade 2 was defined as microperforation and grades 3 and 4 as overt perforation (Fig. 2). Hence, the patients were divided into three groups: (i) no esophageal perforation: group A, (ii) esophageal microperforation: group B, and (iii) overt esophageal perforation: group C. Treatment was selected according to the cause, degree, and location of esophageal perforation. Conservative treatment entailed fasting or a limited diet and antibiotic treatment as needed. Endoscopic interventions or surgical treatment was performed according to the patientŌĆÖs medical condition.
Complications caused by the initial esophageal injury itself was not considered. Therefore, findings observed as signs of perforation on CT at the ED was not included as complications. Complications of esophageal injury included pneumonia, esophageal stricture, esophageal fistula, lung abscess, and peritonitis. Severe mediastinitis that occurred after esophageal injury or worsened during treatment was included as a complication.
We calculated the ratio between each group by analyzing the data frequency obtained through a medical record review. Continuous data are presented as mean┬▒SD or median (interquartile range). Comparison between the three groups was analyzed using the Kruskal-Wallis test, a non-parametric method. To analyze the effect on increasing complication risks, we analyzed possible variables using the chi-square test or FisherŌĆÖs exact test. Multivariate logistic regression analysis was performed with variables that had obtained P<0.20 in the univariate analysis. The results obtained in the analysis were organized into OR, 95% CI, and P values. Statistical significance was set at P<0.05. All statistical analyses were performed using SPSS (version 25.0; IBM Corp., Chicago, IL, USA).
A total of 1,423 patients who visited the ED for esophageal injury were enrolled initially. Among them, 695 patients underwent CT in the ED and 281 were hospitalized with suspected esophageal injury (Fig. 1). Patients were classified into three groups according to the degree of perforation. Group A included 223 patients (79.4%), group B included 20 patients (7.1%), and group C included 38 patients (13.5%) (Table 1).
The mean age at presentation was 54.2┬▒16.7 years and 159 patients (56.6%) were female. Patients with overt perforation were predominantly males (63.2%, n=24) than females (36.8%, n=14). There were no significant differences in the median age among the three groups (56.0 [42.0~63.0], 53.0 [39.0~63.5], 57.5 [47.0~70.0] years in group A, B, and C, respectively, P=0.367). Group C had the highest percentage of patients over the age of 65 years (36.8%, n=14), followed by group A (22.9%, n=51) and group B (20.0%, n=4).
In all groups, foreign body ingestion (82.9%, n=233) was the most common cause of perforation, followed by chemical injuries (6.4%, n=18) and Boerhaave syndrome (5.0%, n=14). The perforation location was classified as cervical (19.0%, n=11), thoracic (74.1%, n=43), and abdominal (6.9%, n=4). The thoracic region was the most common perforation site.
The mean WBC and CRP values measured at the initial ED visits were higher than the normal range only in group C (P<0.001 for both WBC and CRP values). The time-to-diagnosis was the longest in group C, with a median value of 24 hours (6.0~72.0), followed by 6.5 hours (2.3~42.0) and 2.0 hours (1.0~10.4) in groups B and A, respectively (P<0.001).
The therapeutic method was analyzed differently according to the degree of perforation. In group B, most patients were managed conservatively (50.0%, n=10), followed by endoscopic manipulation (35.0%, n=7) and surgical management (15.0%, n=3). Most patients in group C were treated surgically (52.7%); five patients (13.2%) underwent otolaryngology surgery, 15 patients (39.5%) underwent cardiothoracic surgery (CS) with general surgery (GS), and five patients (13.2%) underwent endoscopic clipping after foreign body removal.
In group B, otolaryngology surgery and foreign body removal was performed through a rigid endoscope. In group C, neck exploration or abscess incision and drainage was performed. Most CS surgeries involved primary closures using thoracotomy. The most common GS surgery was esophagectomy with total gastrectomy and jejunal or colonic interposition.
Complications were pneumonia, esophageal fistula, esophageal stricture, lung abscess, peritonitis, and severe mediastinitis. Five patients (2.2%) developed complications in group A, four patients (20.0%) in group B, and 15 patients (39.5%) in group C. These indicate that the more severe the perforation, the more complications occurred (Table 2).
Among the complications, pneumonia occurred most frequently, followed by esophageal stricture, esophageal rupture, severe mediastinitis, lung abscess, and peritonitis. For esophageal stricture, endoscopic balloon dilatation was performed in two patients in group A, one in group B, and one in group C. No surgical complication occurred after balloon dilatation. Surgical treatment with esophagogastrectomy and colon interposition or feeding jejunostomy were performed in other three patients. In cases of esophageal fistula, primary closure or esophagogastrectomy with interposition, was performed. Severe infection, such as pneumonia, mediastinitis, lung abscess, and peritonitis, was treated with antibiotics.
The main causes of esophageal injury were different for each complication. The most common cause of pneumonia was foreign bodies, followed by Boerhaave syndrome and chemical injury. Esophageal stricture was most caused by chemical injury, followed by Boerhaave syndrome. On the other hand, for esophageal fistula, Boerhaave syndrome was the most common cause, followed by foreign bodies. Besides, both severe mediastinitis and lung abscesses were mostly caused by foreign bodies, and peritonitis was mostly caused by chemical injuries.
Four patients died of complications: one patient (5.0%) in group B and three patients (7.9%) in group C (Table 1). One patient in group B who received primary closure for microperforation due to Boerhaave syndrome, eventually died of acute respiratory distress syndrome (ARDS) during treatment. The clinical courses of three deceased patients in group C were as follows: (i) corrosive injury caused by pesticides, resulted in aggravation of pneumonia during postoperative treatment and death, (ii) vomiting led to Boerhaave syndrome, resulting in pneumonia during conservative treatment and progression to ARDS and death, and (iii) esophageal perforation caused by a foreign body (crab), and pneumonia progressed during the postoperative period and death.
The risk factors for esophageal perforation-related complications in patients who visited the ED have been organized in Table 3. In the univariate analysis, male sex, age Ōēź65 years, chronic liver disease, and cerebrovascular disease were associated with a high risk of perforation-related complications. Patients with Boerhaave syndrome and chemical injuries had a high risk of complications. Among the CT grades, the risk of complications was high in those with grade 4. In a multivariate analysis the following variables were associated with a significant risk for complications: age Ōēź65 years (OR 4.14, 95% CI 1.18~14.56, P=0.027), cerebrovascular disease (OR 8.58, 95% CI 1.13~65.19, P=0.038), Boerhaave syndrome (OR 12.52, 95% CI 2.07~75.68, P=0.006), chemical injury (OR 15.72, 95% CI 3.67~67.28, P<0.001), and CT grade 4 (OR 15.75, 95% CI 4.39~56.55, P<0.001).
Esophageal perforation is a rare, but potentially lethal, clinical condition. Therefore, the evaluation of risk factors and its clinical application in treatment planning are important [4,7]. In the present study, initial CT scanning detected overt perforation in 13.5% of hospitalized patients presenting with esophageal injury to the ED, and microperforation in 7.1%. Initial CT grading and risk stratification assessment in patients with esophageal injury visiting the ED was undertaken for definitive management; 20.7% (n=12) of patients with perforation (n=58) underwent endoscopic treatment, and 39.7% (n=23) of patients with perforation underwent surgical treatment. Among patients with esophageal injury who visited the ED, complications occurred in 8.5% (n=24) of all patients, and 1.4% (n=4) died. Risk factors for esophageal injury-related complications were age Ōēź65 years, cerebrovascular disease history, and esophageal damage caused by Boerhaave syndrome or chemicals.
In previous studies regarding patients with esophageal injury during hospitalization, procedure-related iatrogenic injury was the leading cause of esophageal perforation, especially in the Western countries [1,11,12]. In the present study, the main cause of esophageal injury was a foreign body, because it was conducted in an Asian country where fish and chicken are eaten on bone [13]. However, in foreign body-related esophageal injuries, the possibility of complications was relatively low (OR 0.09, 95% CI 0.04~0.22). In patients with foreign body-related injuries without microperforation or overt perforation, endoscopic management is an effective and safe therapeutic modality. However, chemical injury caused by acid or alkali indigestion and Boerhaave syndrome, usually related to heavy alcohol use, resulted in more serious complications; these causes are relatively rare in the Western study [13].
Determining the esophageal injury severity in the ED is important to identify at-risk patients and optimize management. Therefore, the initial risk stratification is important. CT findings can indicate the presence of esophageal perforation and predict the need for endoscopic or other surgical interventions. Furthermore, a delayed perforation diagnosis may be related to the occurrence of complications and mortality. Therefore, CT scan plays a crucial role in identifying patients with perforations or other complications that require surgical intervention. Clinical presentation and simple radiology are not reliable enough, especially in cases of fish bone-related perforation [14]. In adult patients with symptomatic fish bones impaction, the sensitivity of plain X-ray is 32%; the sensitivity of CT scans is 90~100% and specificity is 93.7~100% [14-16]. There is a four-stage CT classification based on transmural necrosis in esophageal caustic injuries; owing to the absence of post-contrast wall enhancement, which is a good indicator of long-term outcomes [10,17]. To the best of our knowledge, there is no CT grading system to estimate the extent of esophageal injury, including corrosive injury, and to predict the prognosis in an ED setting. The present study demonstrated that CT grading is a good predictor of the complication risks and outcomes in patients with esophageal injury.
Emergency endoscopy is vital in the diagnosis and management of esophageal injuries. In the present study, conservative treatment was commonly employed in cases of microperforation on the initial CT, followed by endoscopic treatment. Several existing studies have demonstrated the effectiveness of endoscopic treatment for microperforation [18,19]. The European Society for Gastrointestinal Endoscopy recommends endoscopic treatment for esophageal and gastric perforations using clips or other devices, particularly for perforations <10 mm in size [20]. We performed endoscopic clipping for esophageal perforations of approximately 1.0 cm-size. We started with the normal mucous membrane under the perforation which were pulled and clipped on both sides, and gradually the perforation site was ligated using the suture (Fig. 3). Apart from these technical aspects, the timing of endoscopic procedures is also significant [8]. If inflammation occurs without proper treatment for perforations, endoscopic clipping may fail because of damage to the tissue surrounding the perforation. Therefore, determining the treatment modality based on the initial CT is important for predicting the outcomes.
The strength of this study is that it included a homogenous sample of patients with esophageal injury who visited the ED. Our results indicate that early CT evaluation is important when a patient with an esophageal injury visits the ED owing to the high risk of complications. These possible predictors could help to explain the prognosis of patients. The present study had some limitations. First, this study was conducted retrospectively, which could have caused a selection bias. It is highly likely that patients with a low risk of complications were excluded from the analysis even if they visited the emergency room with esophageal damage because CT scan was omitted. Second, this study was conducted at a referral center; therefore, the results may not be applicable to general physicians. Further multicenter studies are necessary for large-scale surveys. Third, we did not analyze the cost-effectiveness of CT scans. CT scans are expensive and have radiological hazards; however, without it, perforation-related complications can result in mortality. Thus, further analysis on cost-effectiveness is needed.
In conclusion, initial screening and CT grading in the ED play a significant role in predicting potential complication and determining management strategies in esophageal injury patients with suspected perforation. Therefore, we recommend CT for high-risk patients with clinical suspicion of perforation or situations that might secondarily lead to perforation in the ED setting. Initial CT grading and assessment of risk stratification in patients presenting with esophageal injury to the ED are useful for managements at emergent conditions.
Fig.┬Ā1.
Flow chart showing inclusion and exclusion criteria used in the study. ED, emergency department.

Fig.┬Ā2.
CT criteria for grading of esophageal perforation. (A) Normal CT image (grade 1). (B) Pneumomediastinum with microperforation (grade 2, yellow arrow). (C) Severe mediastinitis with overt perforation (grade 3, yellow arrow). (D) Severe left hydropneumothorax (right yellow arrow) with overt perforation (left yellow arrow) (grade 4).
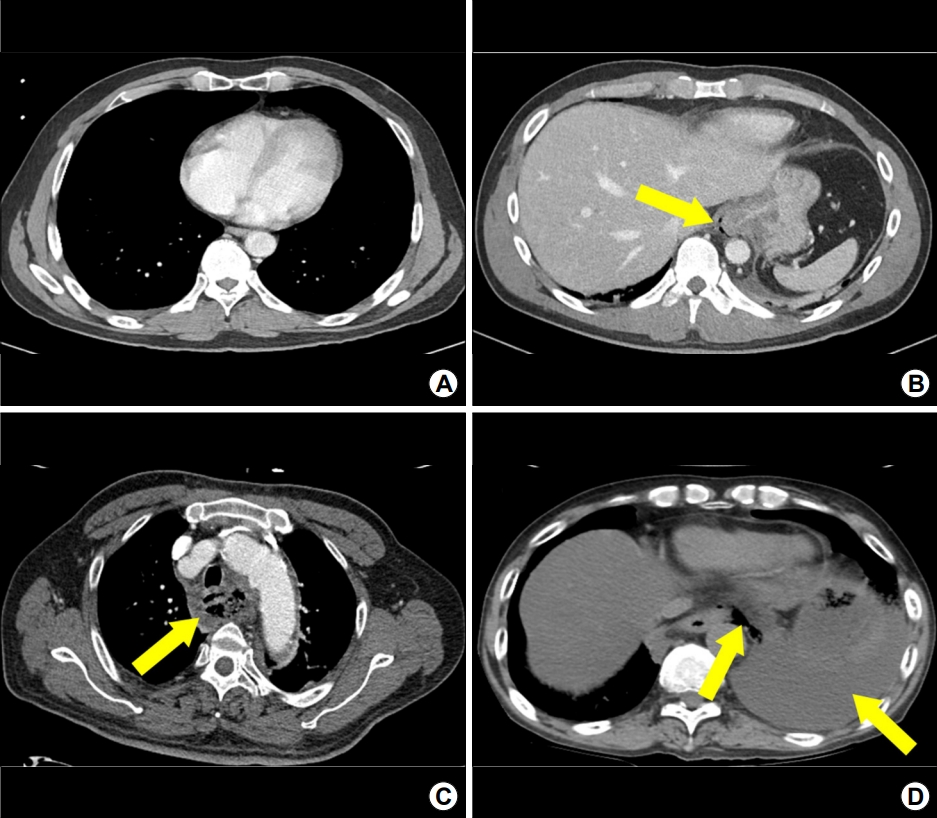
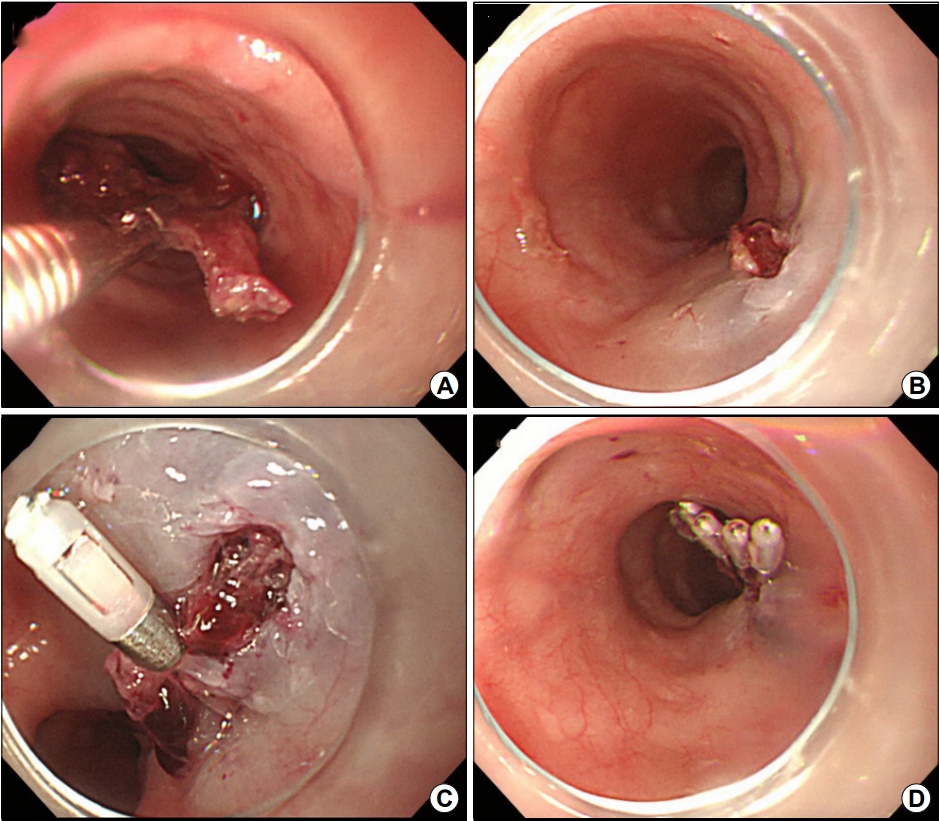
Fig.┬Ā3.
Endoscopic management of esophageal perforation. (A) Image showing removal of foreign body (fishbone) using endoscopic alligator forceps. (B) Overt perforation is observed after foreign body removal. (C, D) Esophageal perforation is sealed off using endoscopic clipping to avoid further surgical management.
Table┬Ā1.
Baseline Characteristics of Patients with Esophageal Injury
| No perforation (n=223) | Microperforation (n=20) | Overt perforation (n=38) | P-value | ||
|---|---|---|---|---|---|
| Sex | |||||
| Male | 87 (39.0) | 11 (55.0) | 24 (63.2) | ||
| Female | 136 (61.0) | 9 (45.0) | 14 (36.8) | ||
| Agea | 56.0 (42.0~63.0) | 53.0 (39.0~63.5) | 57.5 (47.0~70.0) | 0.367 | |
| Ōēź65 years | 51 (22.9) | 4 (20.0) | 14 (36.8) | ||
| Comorbidities | |||||
| HTN | 48 (21.5) | 4 (20.0) | 8 (21.1) | ||
| DM | 22 (9.9) | 2 (10.0) | 2 (5.3) | ||
| Cardiac disease | 10 (4.5) | 1 (5.0) | 2 (5.3) | ||
| Liver disease | 4 (1.8) | 0 (0.0) | 4 (10.5) | ||
| Renal disease | 1 (0.4) | 0 (0.0) | 0 (0.0) | ||
| Lung disease | 6 (2.7) | 1 (5.0) | 2 (5.3) | ||
| Cerebrovascular disease | 7 (3.1) | 1 (5.0) | 2 (5.3) | ||
| Cause | |||||
| Foreign body | 196 (87.9) | 16 (80.0) | 21 (55.3) | ||
| Chemical injury | 15 (6.7) | 0 (0.0) | 3 (7.9) | ||
| Boerhaave syndrome | 2 (0.9) | 4 (20.0) | 8 (21.1) | ||
| Trauma | 8 (3.63) | 0 (0.0) | 3 (7.9) | ||
| Iatrogenic | 2 (0.9) | 0 (0.0) | 2 (5.3) | ||
| Abscess | 0 (0.0) | 0 (0.0) | 1 (2.6) | ||
| Perforation site | |||||
| Cervical | 2 (10.0) | 9 (23.7) | |||
| Thoracic | 18 (90.0) | 25 (65.8) | |||
| Abdominal | 0 (0.0) | 4 (10.5) | |||
| Initial WBC (103/╬╝L)a,b | 6.5 (5.5~8.7) | 9.4 (6.4~12.1) | 11.6 (7.2~15.2) | <0.001 | |
| Initial CRP (mg/dL)a,c | 0.1 (0.0~0.2) | 0.2 (0.1~1.5) | 2.1 (0.3~16.4) | <0.001 | |
| Time to diagnosis (hours)a | 2.0 (1.0~10.4) | 6.5 (2.3~42.0) | 24.0 (6.0~72.0) | <0.001 | |
| Treatment | |||||
| Endoscopic treatment | 142 (63.7) | 7 (35.0) | 5 (13.2) | ||
| Conservative treatment | 65 (29.2) | 10 (50.0) | 13 (34.2) | ||
| Surgery (otolaryngology) | 14 (6.3) | 1 (5.0) | 5 (13.2) | ||
| Surgery (CS, GS) | 2 (0.9) | 2 (10.0) | 15 (39.5) | ||
| Complications | 5 (2.2) | 4 (20.0) | 15 (39.5) | ||
| Mortality | 0 (0.0) | 1 (5.0) | 3 (7.9) | ||
Table┬Ā2.
Comparison of Complications between the Esophageal Injury Groups
Table┬Ā3.
Risk Factors Associated with Complications in Patients Presenting to the Emergency Department with Esophageal Injuries
|
Univariable analysis |
Multivariable analysis |
||||||
|---|---|---|---|---|---|---|---|
| OR | 95% CI | P-value | OR | 95% CI | P-value | ||
| Sex | |||||||
| Male | 1.931 | 0.827~4.512 | 0.123 | 0.530 | 0.148~1.896 | 0.329 | |
| Female | 1 (reference) | ||||||
| Age | |||||||
| Ōēź65 years | 4.242 | 1.803~9.982 | <0.001 | 4.144 | 1.179~14.564 | 0.027 | |
| <65 years | 1 (reference) | ||||||
| Comorbidity | |||||||
| HTN | 1.253 | 0.474~3.310 | 0.648 | ||||
| DM | 2.136 | 0.531~5.280 | 0.256 | ||||
| Cardiac disease | 0.910 | 0.877~0.945 | 0.612 | ||||
| Liver disease | 3.803 | 0.724~19.973 | 0.143 | 2.115 | 0.172~26.035 | 0.559 | |
| Lung disease | 0.912 | 0.879~0.946 | 1.000 | ||||
| Cerebrovascular disease | 5.102 | 1.228~21.191 | 0.044 | 8.575 | 1.128~65.186 | 0.038 | |
| None | 1 (reference) | ||||||
| Cause | |||||||
| Foreign body | 0.088 | 0.036~0.218 | <0.001 | ||||
| Boerhaave syndrome | 14.706 | 4.623~46.775 | <0.001 | 12.518 | 2.071~75.679 | 0.006 | |
| Chemical injury | 9.209 | 3.166~26.780 | <0.001 | 15.721 | 3.673~67.281 | <0.001 | |
| Trauma | 0.911 | 0.878~0.946 | 0.607 | ||||
| Iatrogenic | 0.913 | 0.881~0.947 | 1.000 | ||||
| None | 1 (reference) | ||||||
| Perforation site | |||||||
| Cervical | 3.803 | 0.724~19.973 | 0.343 | ||||
| Thoracic | 8.163 | 5.460~44.027 | 0.208 | ||||
| Abdominal | 9.591 | 1.557~86.314 | 0.238 | ||||
| None | 1 (reference) | ||||||
| Initial CT gradinga | |||||||
| Grade 1 | 1 (reference) | ||||||
| Grade 2 | 3.013 | 0.919~9.871 | 0.278 | ||||
| Grade 3 | 2.830 | 0.566~14.151 | 0.206 | ||||
| Grade 4 | 19.067 | 7.319~49.669 | <0.001 | 15.752 | 4.388~56.547 | <0.001 | |
| Time to diagnosis (hours) | 1.005 | 1.001~1.010 | 0.225 | ||||
REFERENCES
2. Hasimoto CN, Cataneo C, Eldib R, et al. Efficacy of surgical versus conservative treatment in esophageal perforation: a systematic review of case series studies. Acta Cir Bras 2013;28:266ŌĆō271.


3. Carrott PW Jr, Low DE. Advances in the management of esophageal perforation. Thorac Surg Clin 2011;21:541ŌĆō555.


4. Chirica M, Kelly MD, Siboni S, et al. Esophageal emergencies: WSES guidelines. World J Emerg Surg 2019;14:26.




5. Addas R, Berjaud J, Renaud C, Berthoumieu P, Dahan M, Brouchet L. Esophageal perforation management: a single-center experience. Open J Thorac Surg 2012;2:111ŌĆō117.


6. Keeling WB, Miller DL, Lam GT, et al. Low mortality after treatment for esophageal perforation: a single-center experience. Ann Thorac Surg 2010;90:1669ŌĆō1673.


7. Zimmermann M, Hoffmann M, Jungbluth T, Bruch HP, Keck T, Schloericke E. Predictors of morbidity and mortality in esophageal perforation: retrospective study of 80 patients. Scand J Surg 2017;106:126ŌĆō132.



8. Biancari F, DŌĆÖAndrea V, Paone R, et al. Current treatment and outcome of esophageal perforations in adults: systematic review and meta-analysis of 75 studies. World J Surg 2013;37:1051ŌĆō1059.



9. Ruan WS, Li YN, Feng MX, et al. Retrospective observational analysis of esophageal foreign bodies: a novel characterization based on shape. Sci Rep 2020;10:4273.




10. Chirica M, Bonavina L, Kelly MD, Sarfati E, Cattan P. Caustic ingestion. Lancet 2017;389:2041ŌĆō2052.


11. Vallb├Čhmer D, H├Člscher A, H├Člscher M, et al. Options in the management of esophageal perforation: analysis over a 12-year period. Dis Esophagus 2010;23:185ŌĆō190.


12. Kang DH, Ryu DG, Choi CW, et al. Clinical outcomes of iatrogenic upper gastrointestinal endoscopic perforation: a 10-year study. BMC Gastroenterol 2019;19:218.




13. Liao F, Zhu Z, Pan X, et al. Safety and efficacy of nonoperative treatment in esophageal perforation caused by foreign bodies. Clin Transl Gastroenterol 2022;13:e00451.



14. Goh BK, Tan YM, Lin SE, et al. CT in the preoperative diagnosis of fish bone perforation of the gastrointestinal tract. AJR Am J Roentgenol 2006;187:710ŌĆō714.


15. Young CA, Menias CO, Bhalla S, Prasad SR. CT features of esophageal emergencies. Radiographics 2008;28:1541ŌĆō1553.


16. Ngan JH, Fok PJ, Lai EC, Branicki FJ, Wong J. A prospective study on fish bone ingestion. Experience of 358 patients. Ann Surg 1990;211:459ŌĆō462.


17. Ryu HH, Jeung KW, Lee BK, et al. Caustic injury: can CT grading system enable prediction of esophageal stricture? Clin Toxicol (Phila) 2010;48:137ŌĆō142.


18. Romero RV, Goh KL. Esophageal perforation: continuing challenge to treatment. Gastrointest Interv 2013;2:1ŌĆō6.








