Dilation of the Duodenal Limb after Resection of a Huge Jejunal Gastrointestinal Stromal Tumor
Article information
Question: A 70-year-old woman presented with right upper quadrant pain and vomiting. Six months before, she had underwent segmental resection of a huge 13 cmsized gastrointestinal stromal tumor in the proximal jejunum and gastrojejunostomy (Fig. 1A). On abdominal CT at visit, marked dilation of the excluded duodenal limb (from the gastric pylorus to the transected distal duodenum) was observed (Fig. 1B).

(A) Abdominal computed tomography (CT) at the time of segmental resection and gastrojejunostomy (6 months prior) showing a huge 13-cm-sized gastrointestinal stromal tumor in the proximal jejunum. (B) Abdominal CT at hospital visit revealing marked dilation of the excluded duodenal limb (asterisk, from the gastric pylorus to the transected distal duodenum).
What is the appropriate treatment?
Answer: Because the duodenal limb dilation was thought to be caused by closed loop formation secondary to the intact pyloric function, endoscopic pyloromyotomy was planned. After submucosal injection of a saline solution mixed with diluted epinephrine (0.025 mg/mL) and indigo carmine, a mucosal incision was made in the posterior wall of the gastric antrum, 5 cm proximal to the pylorus (Fig. 2A). Then, a submucosal tunnel was created from the mucosal entry to approximately 1 cm over the pylorus (Fig. 2B). Full-thickness myotomy was performed from 2 cm proximal to the pylorus to 1 cm beyond the pylorus (Fig. 2C). Thereafter, the mucosal entry was closed with metal clips and a detachable snare (Fig. 2D). The next day her symptoms improved and then discharged 3 days later. At 25 months follow-up, no recurrence of symptoms was noted.
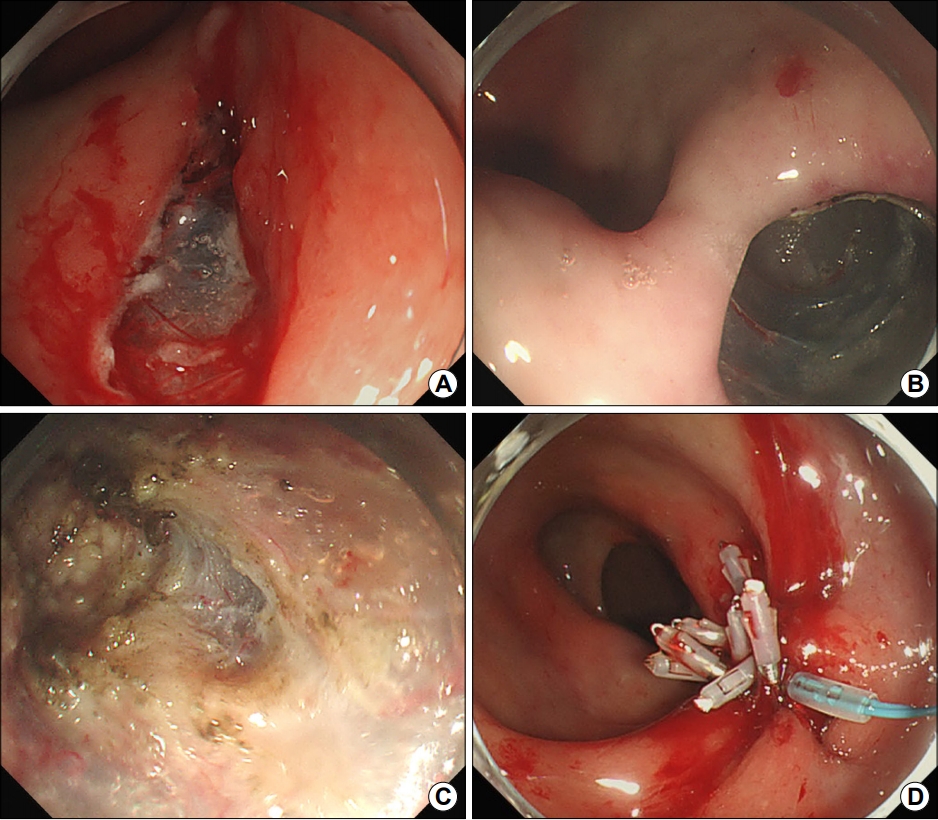
(A) Creation of a mucosal incision in the posterior wall of the gastric antrum 5 cm proximal to the pylorus. (B) Creation of a submucosal tunnel from the mucosal entry to approximately 1 cm beyond the pylorus. (C) Performance of full-thickness myotomy from 2 cm proximal to the pylorus to 1 cm beyond the pylorus. (D) Closing of the mucosal entry with metal clips and a detachable snare.
As one of the submucosal endoscopies, peroral endoscopic myotomy is known as one of the safe and efficient treatment modalities for esophageal achalasia with a higher clinical outcomes success rate over 90% [1]. This technique can be also adopted to other functional gastrointestinal disorders, including gastroparesis. In recent decade, gastric peroral endoscopic pyloromyotomy has been widely explored as a pylorus-directed therapy for gastroparesis [2].
In the excluded duodenal limb dilation caused by the intact pylorus, mechanical or functional disruption of the pyloric muscle can be one of treatment options. Disruption of the pyloric muscle is possible by surgical pyloroplasty, transpyloric stenting, or intrapyloric botulinum injection [3]. Similarly to esophageal achalasia, endoscopic pyloromyotomy can be a substitute to the surgical pyloroplasty in the excluded duodenal limb dilation caused by the intact pylorus.
Notes
No potential conflict of interest relevant to this article was reported.
