A Mass in the Stomach Observed after Endoscopic Ultrasonography-guided Fine-needle Aspiration for Pancreatic Cancer
Article information
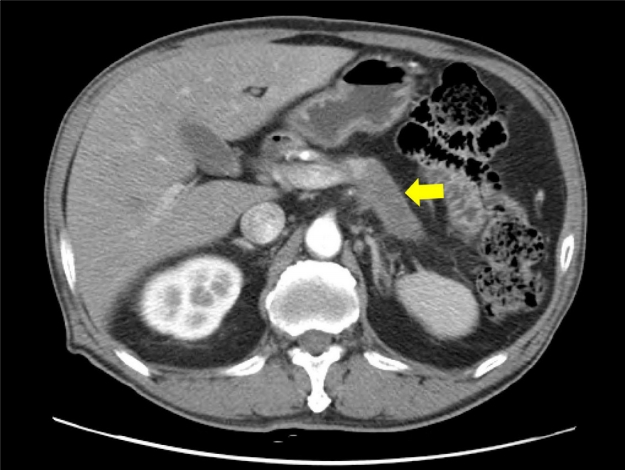
Question: A 68-year-old man underwent EUS-guided fine-needle aspiration (FNA) for a 6.5 cm-sized pancreatic body/tail mass (Fig. 1). EUS-FNA with 4 passes using a 22 G needle was conducted through the upper body of the stomach, and there was no abnormal lesion except minor bleeding in the FNA site (Fig. 2). The diagnosis of pancreatic cancer was confirmed, and the 8th American Joint Committee on Cancer stage was T4N0M0 due to invasion into the celiac artery. Therefore, the patient was administered intravenous chemotherapy (gemcitabine+cisplatin) and remained stable for 6 months. On follow-up upper gastrointestinal endoscopy, a subepithelial tumorlike lesion with central ulceration was detected at the posterior wall of the upper body of the stomach (Fig. 3A). On EUS, the lesion was mainly located in the submucosal layer of the stomach without conglutination to the pancreatic mass (Fig. 3B).

After EUS-guided fine-needle aspiration, no abnormal lesions were observed except for minor bleeding in the upper body of the stomach.
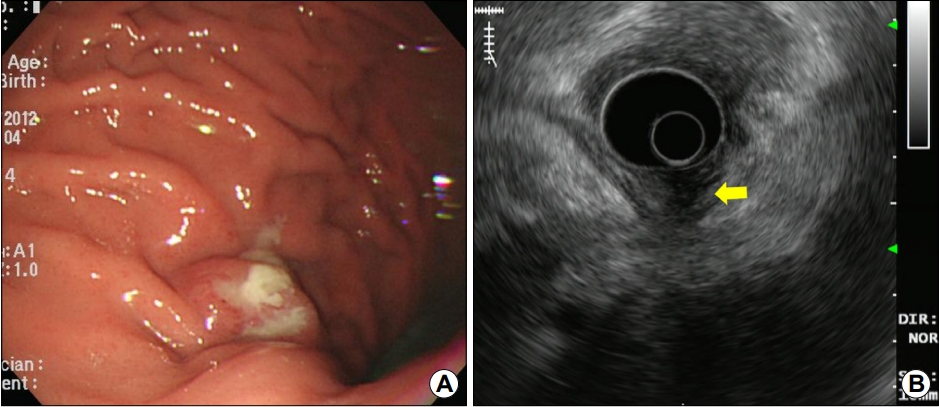
(A) Follow-up endoscopy shows a subepithelial tumor-like lesion with central ulceration at the posterior wall of the upper body of the stomach. (B) EUS shows that the lesion is mainly located in the submucosal layer of the stomach without conglutination to the pancreatic mass (arrow).
What is the most likely diagnosis?
Answer: The endoscopic biopsy specimen obtained from the subepithelial tumor-like lesion revealed adenocarcinoma, pathologically identical to that of primary pancreatic cancer (Fig. 4). Therefore, needle tract seeding of pancreatic cancer into the stomach was diagnosed.
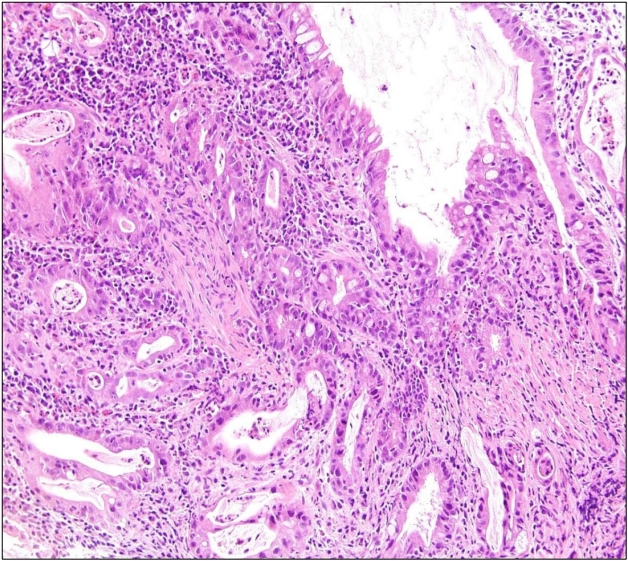
The endoscopic biopsy specimen obtained from the subepithelial tumor-like lesion indicates adenocarcinoma, pathologically identical to that of primary pancreatic cancer (H&E, ×200).
EUS-FNA is a useful and relatively safe diagnostic modality for pancreatic cancer; the adverse event rates are very low (<1% in large centers) and the risks of tumor seeding are lower compared to transcutaneous methods [1]. However, as the number of EUS-FNA increases, the possibility of needle tract seeding occurring after EUS-FNA should always be minded [2]. Especially, in cases when surgical resection does not include the needle tract, such as cancers in the body or tail of the pancreas, EUS-FNA should be cautiously considered and the number of needle passes should be minimized. Close periodical examinations including gastroscopy should be scheduled for patients who undergo EUS-FNA without needle tract resection [3]. In summary, even though needle tract seeding is a rare adverse event of EUS-FNA in pancreatic cancer, it can occur, especially when the cancer is located in the body or tail of the pancreas.
Notes
No potential conflict of interest relevant to this article was reported.