Factors Associated with Belching and Retching during Esophagogastroduodenoscopy and Their Effects on Z-Line Appearance
Article information
Abstract
Background/Aims
Belching and retching tend to cause technical difficulties during endoscopic procedures; however, risk factors associated with belching and retching during endoscopy remain unclear. In this study, we investigated the factors associated with belching and retching during unsedated endoscopy and the effects of belching and retching on the grading of Los Angeles (LA) classification of reflux esophagitis.
Materials and Methods
This prospective observational study included patients who underwent unsedated esophagogastroduodenoscopy (EGD). We used a predefined grading system to evaluate belching and retching during the endoscopic examination. LA classification grades were compared between the endoscope insertion and withdrawal phases of EGD.
Results
The study included 327 patients. Age (specifically, young age [<60 years]) was significantly associated with belching and retching (P<0.001). Belching and retching were not associated with statistically significant change of the LA classification (P=0.962). However, we observed differences in Z-line appearance between the endoscope insertion and withdrawal phases in several patients.
Conclusions
Age was significantly associated with belching and retching during unsedated EGD. Notably, Z-line appearance was also changed during EGD in some patients.
INTRODUCTION
Esophagogastroduodenoscopy (EGD) is a useful diagnostic tool for the evaluation of the upper gastrointestinal (GI) tract [1]. The stomach is dilated by air insufflation into the lumen for detailed visualization of the upper GI tract. Belching is the release of air from the esophagus or the stomach into the pharynx during transient lower-esophageal sphincter relaxation. Retching is strenuous contractions of diaphragm and muscles of the chest and abdominal wall without expulsion of the stomach content [2,3]. Belching and retching are major obstacles that limit detailed examination during unsedated EGD and causes considerable discomfort to the patient and physician [3].
Gastroesophageal reflux disease (GERD) is one of the most commonly encountered conditions in the gastroenterology clinic [4]. Endoscopy is an essential tool for the evaluation and management of patients with GERD that allows identification of the presence of mucosal injuries, such as erosions, ulcers, strictures, and Barret’s esophagus [5]. The esophagogastric junction (EGJ) is a narrow area that can be injured by endoscopic manipulation [6-8]. Experientially, patients often belch and retch during EGD, which may leads to further injury of the esophagus. However, few studies have assessed the effect of endoscopic manipulation, belching and retching on the grading of Los Angeles (LA) classification.
In this prospective observational study, we aimed to investigate the factors associated with belching and retching, and analyze whether belching and retching leads to significant changes in grading of LA classification.
MATERIALS AND METHODS
1. Study population
Patients who were scheduled for EGD at the gastrointestinal endoscopy unit and health promotion center of Kangwon National University Hospital between February 2017 and February 2018 were prospectively included in this study. Patients older than 18 years were enrolled. Patients who underwent unsedated EGD for diagnostic, screening, or surveillance purposes were eligible. Patients who were scheduled for therapeutic interventions, such as bleeding control, foreign body removal, endoscopic submucosal dissection, stent insertion, balloon dilatation were excluded. Other exclusion criteria included inability to cooperate with the EGD procedure, failure to take images of the EGJ properly, and failure to obtain informed consent. Written informed consent was obtained from all the patients. The study was approved by the Institutional Review Board of Kangwon National University Hospital (KNUH 2017-02-007).
2. Data collection
EGD was performed using a conventional video gastroscope (GIF H260, diameter: 9.8 mm or GIF-HQ290, diameter: 10.2 mm; Olympus, Tokyo, Japan) by two experienced endoscopists who performed more than 3,000 upper gastrointestinal endoscopies. During EGD, the severity of belching and retching was assessed as described below. Still images of EGJ were captured during both insertion and withdrawal phases of EGD. If EGJ was poorly visible, Valsalva maneuver was performed to fix and visualize the EGJ. As a result, each subject has two image sets of EGJ, one obtained during insertion of scope and the other during withdrawal of scope after the complete examination of stomach and duodenum. All the image sets of EGJ were mixed randomly, and reviewed by the two independent endoscopists who are unaware of the relationship of mixed image sets. Finally, classifications determined by two reviewers were compared with each other, and for incongruent results, final grading was made by mutual agreement. Data including age, sex, underlying disease, BMI, indications of EGD, procedural time, prior experience of EGD, gastroscope model (GIF-H260 or GIF-HQ290), and LA classification were collected.
3. Definitions of events
Endoscopic grading of esophagitis was defined according to the LA classification as described previously [9]. Grade A was defined as ≥1 mucosal breaks of <5 mm, grade B was defined as >1 mucosal breaks of ≥5 mm that were not continuous between the two folds, grade C was defined as ≥1 continuous breaks occupying <75% of the esophageal circumference, and grade D was defined as ≥1 breaks occupying >75% of the circumference. For minimal change lesions, simplified working definition was adopted as follows: white turbid discoloration and blurring of Z-line [10].
Procedure time was defined as the time interval between the first EGJ image during insertion and the first EGJ image during withdrawal of the endoscope after complete examination of the stomach and the duodenum.
Belching was defined as the forceful expulsion of gas through the mouth. Retching was defined as the sound and movement of vomiting without expulsion of gastric contents. As there are no validated or published scoring systems for belching or retching during endoscopy, belching and retching severity was qualitatively scored by the endoscopist as follows: none, mild (presence of an event that does not compromise the procedure quality), moderate (difficult and prolonged examination procedure due to the event; however, able to complete the examination), and severe (inability to evaluate the upper GI tract completely due to the event). We considered moderate or severe belching/retching as a clinically significant event, because the endoscopic examination becomes difficult from moderate score.
The primary endpoint was the analysis and identification of factors affecting belching and retching, and the secondary endpoint was the analysis of changes in LA classification between the insertion and withdrawal phases during endoscopy.
4. Statistical analysis
Sample size was calculated by G*power 3.1.9.7 (Heinrich-Heine-Universität Düsseldorf, Düsseldorf, Germany). We supposed that the effect size will be 0.5 (medium) and the ratio of ‘none or mild’ to ‘moderate or severe’ belching & retching group will be 4 to 1. Group sample size of 160 in ‘none or mild’ group and 40 in ‘moderate or severe’ group were needed to achieve a power of 80%. and an alpha error of 5%. Pearson's chi-Square or fisher’s exact test was performed for categorical variables, and the t-test was performed for continuous variables. Multiple logistic regression analysis was performed for multivariate analysis. Wilcoxon signed ranks test was performed to compare grades of LA classification between insertion and withdrawal phases. Statistical significance was set at a P-value of <0.05. SPSS software (SPSS 21.0 version for Windows; SPSS Inc, Chicago, IL, USA) was used for statistical analysis.
RESULTS
1. Demographic and clinical characteristics of patients
A total of 339 patients who met the inclusion criteria was enrolled in the study. Eleven patients were excluded due to unclear EGJ images and one was excluded due to incomplete recording of the belching and retching score. The remaining 327 patients were included in the study. The demographic and clinical characteristics of the patients are summarized in Table 1. The study population consisted of 49.8% men and 50.2% women with a mean age of 60 years (range, 17~87) at the time of EGD. Mean BMI was 24.68 kg/m2 (range, 17.0~37.2). The most common indication for EGD was screening for gastric cancer (87.8%), followed by evaluation of gastrointestinal symptoms (7.0%) such as dyspepsia, abdominal pain, or chest discomfort. Belching and retching occurred in 71.3% of the patients during EGD (Table 1).
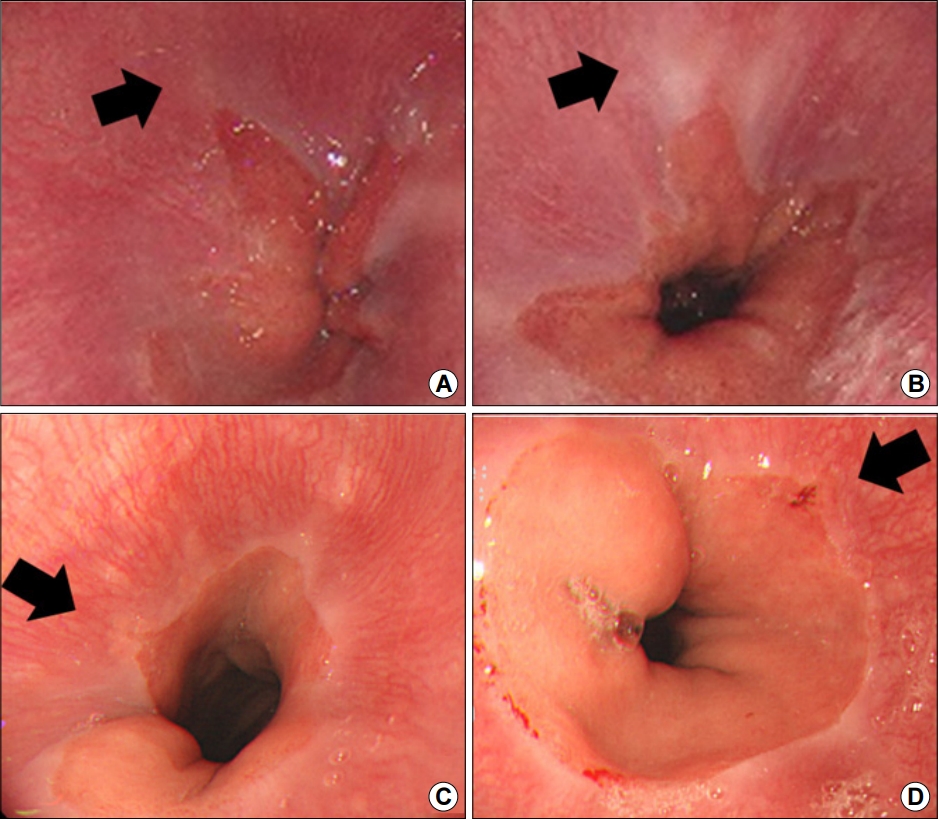
2. Factors associated with belching and retching during unsedated EGD
We analyzed the factors associated with belching and retching as primary outcomes (Tables 2, 3). In the univariate analysis, younger age was significantly associated with belching and retching (P<0.001). More cases of belching and retching were observed in younger patients during EGD. BMI, sex, procedure time, and indications, underlying disease, prior experience of EGD, gastroscope model were Multivariate analysis showed that younger age was the only significant factor associated with belching and retching (P<0.001, Table 3).
3. Association of belching and retching with LA classification changes
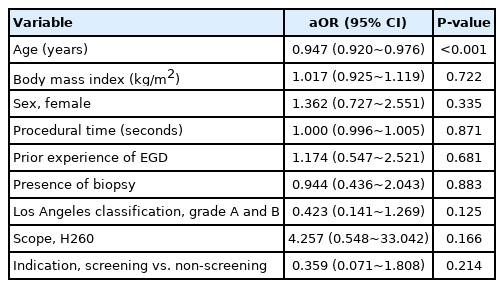
In the insertion and withdrawal phase, there were 108 patients with changes in the LA classification and 219 patients without changes. There was no statistically significant change of LA classification between insertion and withdrawal phase (P=0.494). Among the patients with the change in the LA classification, there were 51 patients majority of changes (77/108, 71%) were from normal to minimal (n=39) or minimal to normal (n=38) classification changes. After reviewing the EG junction image, we have recognized that most changes are not the true change but due to intra- and interobserver variability. However, in some cases, real change of Z-line appearance had occurred (Fig. 1).
Endoscopic images of the esophagogastric junction (EGJ). EGJ images obtained in the same patient during endoscope insertion (A) and withdrawal (B) showing mucosal changes from ‘normal’ to ‘minimal change’ during the procedure. EGJ images obtained in the same patient during endoscope insertion (C) and withdrawal (D) showing mucosal changes from ‘normal’ to ‘grade A’ during the procedure. The black arrow shows the same area during the endoscope insertion and withdrawal phases.
We also analyzed the association between belching and retching during EGD and changes in LA classification. Belching and retching was not associated with LA classification changes between the insertion and withdrawal phases during endoscopy (Table 4).
DISCUSSION
There have been few studies on factors associated with belching and retching during endoscopy. This study investigated the factors affecting belching and retching, and analyzed whether belching and retching leads to significant changes in grading of the LA classification.
Belching, whether as a voluntary or involuntary phenomenon, functions to decompress the stomach and prevent the accumulation of unnecessary air in the intestine [11,12]. Belching is classified into supragastric belching, in which air is artificially sucked in through the contraction of the pharynx or the diaphragm muscle and immediately discharged, and gastric belching, in which gas collects in the stomach and moves through the esophagus [13]. Swallowed air is collected in the proximal portion of the stomach and activates extensor receptors in the proximal gastric wall, which in turn activates the Vagus and diaphragmatic nerves that results in transient lower esophageal sphincter relaxation, which enables venting of gas from the stomach [14-16]. At the same time, the longitudinal muscles of the esophagus and the rectus abdominis muscles are contracted to help gas move from the stomach to the esophagus, and the upper esophageal sphincter relaxation reflex is consequently triggered [17,18]. Transient lower esophageal sphincter relaxation is a period of vagally mediated simultaneous relaxation of the lower esophageal sphincter and the diaphragm angle lasting for 10~60 seconds without swallowing. Its incidence decreases after vagal ganglectomy [19]. There is an overall reduction in autonomic control that integrates and regulates visceral functions to keep homeostasis during changes in external and internal environments with age. Sympathetic tone predominates and vagal tone diminishes with the aging process [20].
Younger age was associated with belching and retching during EGD in univariate and multivariate analysis in this study. A previous study revealed that as age increases, the cognitive ability for stomach distension decreases and the sensory function of the pharynx decreases, resulting in a weaker vomiting reflex [2]. The reason that belching was lower in elderly patients may be due to their lower sensitivity to stimuli.
Also, we analyzed obesity and gender as factors causing belching and retching. Some studies reported that obesity was associated with a significant decrease in lower esophageal sphincter pressure and an increase in transient lower esophageal sphincter relaxation [21]. In addition, it was suggested that central obesity is associated with increased intra-abdominal pressure, which affects belching during endoscopy and GERD [22]. However, in our study, BMI was not significant factor affecting belching and retching severity. Furthermore, we hypothesized that women are more likely to suffer from belching than men due to hypersensitivity to gastric distension and anxiety prior to the procedure. Some studies revealed that women have more severe postoperative pain than men and have a visceral pain threshold [23]. In our study, female had a higher odd ratio for belching and retching than male, but it was not statistically significant.
Several esophagitis grading systems have been developed so far; however, the LA classification is considered the most validated and the most practical system [24,25]. This system has been widely used worldwide since its publication in 1999; however, there is no consensus on the optimal timing of grading during the endoscopy procedure [9]. Furthermore, it is not known whether endoscopic manipulation during EGD can significantly affect the grading of classification. In this study of 327 patients, LA classification was graded during the insertion and withdrawal phases and compared with each other to investigate the effect of endoscopic manipulation on the EGJ appearance and the LA classification. The LA classification system focuses on the size of mucosal breaks, which is defined as an area of slough or erythema with a discrete lined demarcation from the adjacent normal-looking mucosa [9,26]. As shown in Fig. 1, the change of Z-line appearance between insertion and withdrawal phase did occur in some cases resulting in the change of LA classification, even though the statistical significance was not observed.
Our study has the following the strengths and clinical implications. Compared with previous studies, we confirmed how belching and retching affect LA classification. And even if there was no statistically significant effect, LA classification was upgraded in the withdrawal phase than the insertion phase in some cases. It is necessary to consider the effect on belching and retching when observing the Z-line [2,27]. Also, our study can provide useful information about patients who are difficult to perform EGD for endoscopists.
This study has several limitations. First, we did not check GERD symptoms, such as heartburn and regurgitation. Patients with GERD have been reported to belch more frequently during EGD, and the presence of GERD symptoms could be a factor for belching and retching [2]. Second, we did not investigate the patients’ psychological and social factors. One study reported that factors, such as mental stimulation, negative events, life stress, and overwork increase belching and retching [28]. In addition, we did not investigate factors related to increased abdominal pressure such as index of obesity (visceral fat through abdominal pelvic computed tomography, waist circumference) that could affect belching and retching. Third, our study was conducted on patients who visited a single institution for the purpose of endoscopy, which is not an appropriate representation of all patients undergoing endoscopy. Fourth, although the number of patients was calculated by referring to the previous study related to belching, there was limitation in analyzing association between belching, retching and LA classification because patients including LA classification C and D were not registered. Erosive esophagitis of LA-A and LA-B did not differ according to belching and retching in our study.
In conclusion, this study has shown that age is a significant factor associated with belching and retching during unsedated EGD. In particular, more severe belching and retching occurred in younger patients than in the older patients. Even though, belching and retching was not associated with significant LA classification changes between the insertion and withdrawal phases during endoscopy, some patients did show different Z-line appearance. Therefore, when performing unsedated EGD, it might be helpful to pay attention to belching & retching, and observe the Z-line carefully during insertion phase rather than withdrawal phase, especially for young patients undergoing EGD for GERD evaluation
Acknowledgements
This study was supported by 2021 Research Grant from Kangwon National University (520210062).
Notes
No potential conflict of interest relevant to this article was reported.